Weight control and diet
Highlights
Overview- A stable weight depends on a balance between the energy you get from food and the energy you use.
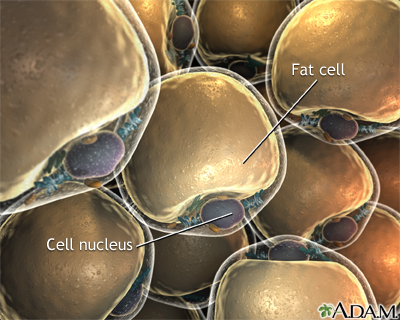
- When a person consumes more calories than the energy they use, the body stores the extra calories in fat cells (lipocytes).
- When a person burns up more calories than they consume, they will lose weight.
- Fat cells grow or shrink depending on how people use energy. If people do not balance energy input and output by eating right and exercising, fat can build up. This leads to weight gain.
- Teaching parents healthy life style skills can lead to a sustained weight reduction in moderately-obese children, even in ethnically diverse populations.
- According to the U.S. Preventive Services Task Force, 17% of children and adolescents (aged 2 - 19) are obese. The prevalence of obesity in America has risen dramatically over the past two decades and continues to increase.
- According to the latest figures available, 35.7% of American adults (aged 20 and older) are obese (BMI 30 and above) -- up from about 23% in the early 1990s.
- A recent study of topiramate in combination with phentermine showed not only sustained weight loss but also metabolic improvements, reducing the risk of diabetes in obese patients.
- The weight loss drug sibutramine (Meridia) has been removed from the market because of a high risk for heart attack and strokes.
- The International Diabetes Federation released a position statement in March 2011, recommending bariatric surgery be considered for patients with Type 2 diabetes and BMI of 30 or greater, if their diabetes does not respond to conventional treatment. Most standard criteria have not recommended weight-loss surgery for diabetics whose BMI is less than 35.
Introduction
A stable weight depends on a balance between the energy you get from food and the energy you use. You use energy during the day in three ways:
- Energy expended during rest (basal metabolism)
- Energy used to break down food (thermogenesis)
- Energy used during physical activity
Basal metabolism accounts for about two-thirds of spent energy. Your body generally uses this energy to keep your temperature steady and the muscles of your heart and intestine working. Thermogenesis accounts for about 10% of spent energy.
When a person consumes more calories than the energy they use, the body stores the extra calories in fat cells (lipocytes). Fat cells function as energy reservoirs. They grow or shrink depending on how people use energy. If people do not balance energy input and output by eating right and exercising, fat can build up. This leads to weight gain.
Measurement of Obesity in Adults
Obesity is determined by measuring body fat, not just body weight. People might be over the weight limit for normal standards, but if they are very muscular with low body fat, they are not obese. Others might be at normal weight or even underweight but still have excessive body fat. The following measurements and factors are used to determine whether or not a person is overweight to a degree that threatens their health:
- Body mass index (BMI) -- a measure of body fat
- Waist circumference (size around the waist)
- Waist-hip ratio
- Skin fold measurement (anthropometry)
A person's disease risk factors and their BMI are important components in determining health risks with weight.
The Body Mass Index (BMI). The current standard measurement for obesity is the body mass index (BMI). In general, a BMI of 25 - 29.9 means you are overweight. Obesity is a BMI of 30 and above. A BMI of 40 or more usually means men are at least 100 pounds over their ideal weight and women are at least 80 pounds over their ideal weight.
Obesity is then classified into three categories:
- Class 1: BMI of 30 - 34.9 (low-risk obesity)
- Class II: BMI 35 - 39.9 (moderate-risk obesity)
- Class III: BMI of 40 and greater (high-risk obesity)
These criteria may be used to estimate the risk for complications of obesity, such as diabetes, heart disease, or certain cancers. They are also used to help decide when surgery may be most appropriate.
Calculating Body Mass Index. A person's body mass index is calculated as follows:
- Multiply one's weight (in pounds) by 703.
- Divide that answer by height in inches.
- Divide that answer again by height in inches.
For example, a woman who weighs 150 pounds and is 5 feet 8 inches (or 68 inches) tall has a BMI of 22.8.
You can check your BMI at the Centers for Disease Control and Prevention BMI calculator.
Waist Circumference Waist measurement is another way to estimate how much body fat a person has. Extra weight around the mid-section or stomach area increases the risk for type 2 diabetes, heart disease, and stroke.
Some studies suggest that:
- Women whose waistlines are over 31.5 inches and men whose waists measure over 37 inches should watch their weight.
- A waist size greater than 35 inches in women and 40 inches in men is associated with a higher risk for heart disease, diabetes, and impaired health.
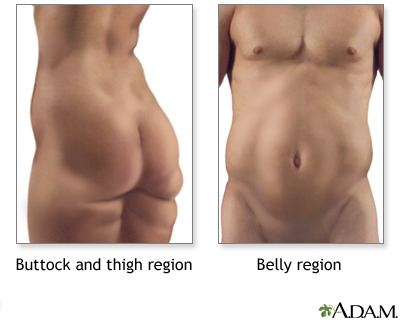
Excess body fat around the abdomen (the "apple-shape") is a more consistent predictor of heart problems and health risks than BMI.
Waist-Hip Ratio. The distribution of fat can be evaluated by dividing waist size by hip size. For example, a woman with a 30-inch waist and 40-inch hip circumference would have a ratio of 0.75; one with a 41-inch waist and 39-inch hips would have a ratio of 1.05. The lower the ratio the better. The risk of heart disease rises sharply for women with ratios above 0.8 and for men with ratios above 1.0.
Anthropometry. Anthropometry is the measurement of skin fold thickness in different areas, particularly around the triceps, shoulder blades, and hips. This measurement is useful in determining how much weight is due to muscle or fat.
Measurement of Obesity in Children
Measuring body fat and diagnosing obesity is different in children and adults.
In children:
- The amount of body fat changes with age. Because of this, a BMI is harder to interpret during puberty and periods of rapid growth.
- Girls and boys normally have different amounts of body fat.
A BMI level that says a child is obese at one age may be normal for a child at a different age. To determine if a child is overweight or obese, experts compare BMI levels of children at the same age to each other. They use a special chart to decide whether a child's weight is healthy or not.
- If a child's BMI is higher than 85% of other children their age and sex, they are considered at risk for being overweight.
- If a child's BMI is higher than 95% of other children their age and sex, they are considered overweight or obese.
Causes
Many people with obesity who lose large amounts of weight and gain it back often think it is their fault. They may blame themselves for not having the will power to keep the weight off, and many regain more than they lost.
Today, we know that biology is the reason some people cannot keep this weight off. Even among people who live in the same environment and eat the same foods, some become obese and others do not. Our bodies have a complex system to help keep weight at a healthy level. In some people, this system may not be working correctly.
Think about the gas gauge in your car. If the gas tank is full but the car's gas gauge is broken, it may read empty. You would want to put in more gas, even when the tank is already full.
Some people may struggle to maintain a healthy weight because one or more of the signals that tells the brain when they have eaten enough does not work correctly. In other words, the gas tank (stomach) may be full, but the brain (gas gauge) does not realize that.
The Biological Pathway to Appetite
Appetite is determined by processes that occur both in the brain and gastrointestinal tract. Eating patterns are controlled by areas in the hypothalamus and pituitary glands (in the brain).
The body produces a number of molecules that increases or decreases appetite, including leptin. Leptin is a hormone that fat cells release. Leptin blood levels rise as the cells store more fat. This increase in leptin levels decreases appetite. Falling levels of leptin make you feel hungry. Still, leptin's role in obesity is unclear.
Specific Genetic Factors
Our bodies are set to maintain weight within a certain range. That weight range is at least partly determined by our genetic makeup. Genetic makeup refers to certain traits that we inherit from our parents. If a person has the genetic makeup for obesity and they eat a lot of high-calorie foods and do not exercise, it is almost certain they will become obese. It will likely be harder for such a person to stay at a healthy weight than someone who does not have the genes for obesity.
Obesity is not caused by just one gene. There are hundreds of genes that influence body weight. Some people have more genetic risk factors for obesity than others. However, scientists have not yet discovered the exact genes that contribute to obesity.
Genetics also determines the number of fat cells a person has. Some people are simply born with more.
Learned Behaviors and Habits
The way we eat when we are children may strongly affect our eating behaviors as adults. When we repeat these behaviors over many years, they become habits. They affect what we eat, when we eat, and how much we eat.
Children are very good at listening to their body's signals of hunger and fullness. They will stop eating as soon as their body tells them they have had enough. However, at some point a well-meaning parent may tell them they have to finish everything on their plate. This forces them to ignore their fullness and to eat everything that is served to them.
As adults, these same people may say that they feel guilty if they do not eat everything on their plate. And today, portion sizes are so large that eating everything on your plate may mean you are eating too many calories.
Other learned behaviors include using food to:
- Reward good behaviors
- Seek comfort when feeling sad or stressed
- Express love
These learned habits lead to eating no matter if someone is hungry or full. Many people have a very hard time breaking these habits.
The foods we eat when we are children may influence our food likes and dislikes for life. Being raised on processed foods that are high in fat, salt, and sugar may make it difficult to start eating natural foods, such as fruits, vegetables, and whole grains, when we become adults. Not knowing how to prepare these foods can also keep people from eating them.
Television and Sedentary Habits
We are surrounded by many things that make it easy to overeat and hard to stay active.
Many people don't have enough time to plan and prepare healthy meals. Some reasons are:
- Having all the adults in a household employed outside the home
- Working longer hours and working evening or night shifts
- Having longer commutes
Less free time also means less time to exercise. Also, more people today work desk jobs compared to jobs in the past that had activity built into them.
Devices such as remote controls, mobile telephones, escalators, elevators, and computers all make life easier for us. But fewer trips up and down stairs and fewer walks down the hall at work to talk with a co-worker mean that we are storing more calories instead of burning them off.
Researchers have found that labor-saving devices had reduced a person's energy use by over 100 calories a day. The average American now eats 100 - 200 more calories a day more than they did 10 years ago. Less activity and more calories can lead to a weight gain of 12 - 25 pounds every year.
Long hours in front of a TV or computer may be the most hazardous pattern of behavior. In one study, TV watching produced a lower metabolic rate than sewing, playing board games, reading, writing, and driving a car. Just the act of watching TV encourages unhealthy snacking and eating patterns.
Modern Diet and Eating Habits
Many things have changed how and what we eat. Some of these are:
- Children see up to 10,000 food commercials every year. Most of these are for candy, fast food, soft drinks, and sugared cereals.
- More foods today are processed and high in fat.
- Vending machines and convenience stores make it easy to get a quick snack, but they rarely sell healthy foods.
- More people eat out, most often at food courts, fast-food restaurants, and all-you-can-eat buffets.
People are not only eating more food than they did 20 years ago but also replacing home cooking with packaged foods, fast food, and dining out. Fast foods may be more harmful than restaurant cooking. These foods tend to be served in larger portions. They generally contain more calories and unhealthy fats, and fewer nutritious ingredients, than homemade or restaurant meals. Snack foods and sweet beverages, including juice and soft drinks, are specific problems that add to the increasing rates of obesity.
Medical or Physical Causes of Obesity
Several medical conditions may contribute to being overweight, but rarely are they a primary cause of obesity.
- Hypothyroidism is sometimes associated with weight gain. But, patients with an underactive thyroid generally show only a moderate weight increase of 5 - 10 pounds.
- Very rare genetic disorders, including Froehlich syndrome in boys, Laurence-Moon-Biedl syndrome, and Prader-Willi syndrome, cause obesity.
- Abnormalities or injury to the hypothalamus gland can cause obesity.
- Cushing's disease is a rare condition caused by high levels of steroid hormones. It results in obesity, a moon-shaped face, and muscle wasting.
- Obesity is also linked to polycystic ovarian syndrome, a hormonal disorder in women.
Effects of Certain Medications
Some prescription medications contribute to weight gain, usually by increasing appetite. Such drugs include:
- Corticosteroids
- Female hormone treatments, including some oral birth control pills (effect is usually temporary), and certain progestins (such as Megestrol) used to treat cancer
- Antidepressants and anti-psychotic drugs, including lithium and valproate
- Insulin and insulin-stimulating drugs used to treat diabetes, a particularly unfortunate conflict of interest for obese individuals with type 2 diabetes
Do NOT stop taking any medications without talking to your health care provider first.
Risk Factors
Where you live plays a role in your risk for obesity. Simply living in the United States makes a person more susceptible to obesity. The prevalence of obesity in America has risen dramatically over the past few years and continues to increase.
- According to the latest figures available more than a third of American adults (ages 20 and older) are obese (BMI over 30) -- up significantly from the early 1990s.
- The number of Americans aged 20 - 74 who were overweight or obese also increased from below 50% in 1960 to 68.0% in 2008.
Risk by Age. People of any age are at risk for obesity. More children and adolescents are overweight in America than ever before. Gaining some weight is common with age, and adding about 10 pounds to a normal base weight over time is not harmful. The typical weight gain in American adults over 50, however, is worrisome. By age 55, the average American has added nearly 40 pounds of fat during the course of adulthood. This condition is made worse by the fact that muscle and bone mass decrease with age.
Risk by Gender. In men, BMI tends to increase until age 50 and then it levels off. In women, weight tends to increase until age 70 before it plateaus. There are three high-risk periods for weight gain in women:
- The first is at the onset of menstruation, particularly if it is early.
- The second is after pregnancy, if weight that has been gained is not lost.
- Finally, many women gain 12 - 15 pounds after menopause.
Risk by Economic Group. Obesity is more prevalent in lower economic groups. Low income women and their families tend to have fewer fruits and vegetables and are actually taking in more calories a day than higher-income women. However, obesity is increasing in young adults with college education as well as in other groups.
Ethnic Groups. Among ethnic groups in general, African-American women are more overweight than Caucasian women are, but African-American men are less obese than Caucasian men are. Hispanic men and women tend to weigh more than Caucasians.
US Regions. Regionally, the prevalence of obesity is lowest in the Western states and highest in the South.
Dietary Habits that Increase Risk
In many cases, lifestyle habits and patterns are so well-established and automatic that people are not even aware that they are bad for health.
A number of dietary habits put people at risk for becoming overweight:
- Night-eating syndrome is defined as having no appetite in the morning, having insomnia, and consuming more than half of the daily food intake after 6 p.m. It is associated with obesity and is difficult to treat.
- About 30% of people who are obese are binge eaters who typically consume 5,000 - 15,000 calories in one sitting Bulimia is binge eating followed by purging in order to lose weight.
Specific Groups at Risk
Anyone with Sedentary Lifestyles. Office workers, drivers, and people who sit for long periods are at higher risk for obesity.
Ex-Smokers. Nicotine increases the metabolic rate, and quitting, even without eating more, can cause weight gain. Most people who quit smoking gain 4 - 10 pounds in the first 6 months after quitting. Some gain as much as 25 - 30 pounds. It is important to note that weight control is not a valid reason to smoke.
People with Disabilities. Obesity rates are higher than average in people with physical or mental disabilities. Those with disabilities in the lower part of the body, such as the legs, are at highest risk.
People with Chronic Mental illnesses. People who have a chronic mental illness are at high risk for obesity and diabetes, most likely due to their lifestyle. In addition, many of the medications used to treat chronic mental illnesses can cause weight gain and increase the risk of diabetes.
Overweight Children: Special Considerations
Obesity has become a serious health problem in children and teenagers. A child who is overweight or obese is more likely to be overweight or obese as an adult.
Obese children are now developing health problems that used to be seen only in adults. When these problems begin in childhood, they often become more severe when the child becomes an adult.
Data from the National Health and Nutrition Examination Survey shows that 17% of children and adolescents (aged 2 - 19) are obese. The number of obese children and adolescents has more than tripled since the 1980s.
No single factor or behavior causes obesity. Obesity is caused by the many factors described above, including a person's habits, lifestyle, and environment. Genetics and some medical conditions also increase a person's chances of becoming obese.
Children are surrounded by many things that make it easy to overeat and harder to be active:
- Parents have less time to plan and prepare healthy meals. As a result, children are eating more processed and fast foods that are usually less healthy than home-cooked meals.
- Vending machines and convenience stores make it easy to get a quick snack, but they rarely sell healthy foods.
- Overeating is a habit that is reinforced by restaurants that advertise high-calorie foods and large portion sizes at low cost
Biological Effect of Childhood Obesity on Adult Weight
Achieving a healthy weight becomes more difficult as children get older. The odds of obesity persisting into adulthood range from 20% in 4 year olds to 80% in teenagers. One reason for the persistence is biological. The fat cells change in number or mass depending on a person's age:
- Fat cells themselves multiply during two growth periods: early childhood and adolescence. Overeating during those times increases the number of fat cells. Some people are also just born with more fat cells.
- After adolescence, fat cells tend to increase in mass rather than quantity, so that adults who overeat and gain weight tend to have larger fat cells, not more of them. This growth in mass may be responsible for the greater risk of persistent obesity among teenagers compared to small children who are overweight. Losing weight after adolescence reduces the size of the fat cells but not their number, so weight loss becomes much more difficult.
Complications
Obesity is a medical condition in which a high amount of body fat makes it hard for a person's internal organs to work well. This can cause poor health. People with obesity are at risk for developing a number of health problems.
Three things can be used to determine if a person's body fat puts them at risk for developing obesity-related diseases:
- Body mass index (BMI)
- Waist size
- Other risk factors or chronic diseases the person has
The higher the BMI, the greater the risk for certain diseases, such as heart disease, stroke, high blood pressure, type 2 diabetes, sleep apnea (pauses in breathing during sleep), and arthritis.
The risk of heart disease rises sharply for women with waist-hip ratios above 0.8 and for men with ratios above 1.0.

General Adverse Effects of Being Overweight (Not Obese). It is still not clear if being overweight (a BMI of 25 - 29.9) harms healthy people with no risk factors for serious illnesses.
The risk for developing diabetes, gallstones, hypertension, heart disease, stroke, and various cancers rises according to how much an individual is overweight. In any case, adults who are overweight in middle age face a poor quality of life as they age, with the quality declining the more they weigh.
Some argue, in fact, that unhealthy diet and sedentary lifestyle cause the harm -- not the extra weight itself -- in people who are not severely obese.
Heart Disease and Stroke
People who are obese have almost three times the risk for heart disease as people with normal weights. Being physically unfit adds to the risk.
As mentioned above, weight concentrated around the abdomen and in the upper part of the body (apple shape) is more commonly associated with insulin resistance and diabetes, high blood pressure, and unhealthy cholesterol and lipid levels.
As a result, obesity poses many dangers to the heart and circulatory system:
- Coronary artery disease and heart attacks
- Heart Failure
- Stroke
Fat that settles in a pear shape around the hips and lower body appears to have a lower association with these conditions:
- High blood pressure
- Unhealthy cholesterol and lipid levels
Insulin Resistance, Type 2 Diabetes, and Metabolic Syndrome
Type 2 Diabetes and Insulin Resistance. Most people with type 2 diabetes are overweight or obese, and weight loss may be the key to controlling the current epidemic of type 2 diabetes. The common factor appears to be insulin resistance -- that is, the body can no longer respond properly to insulin. This has the effect of increasing sugar levels in the blood, the hallmark of diabetes.
Insulin resistance is also associated with high blood pressure and abnormalities in blood clotting. Some research indicates that obesity, in fact, is the one common element linking insulin resistance, type 2 diabetes, and high blood pressure.
Metabolic Syndrome. Metabolic syndrome (also called syndrome X) is a pre-diabetic condition that is significantly associated with heart disease and higher mortality rates from all causes. The syndrome consists of obesity marked by abdominal fat, unhealthy cholesterol levels, high blood pressure, and insulin resistance.
Cancer
The American Cancer Society's (ACS) cancer prevention guidelines stress the importance of keeping a healthy weight throughout life. The ACS indicates that healthy weight is even more important than eating specific healthy foods, when it comes to cancer prevention.
Obesity has been associated with a higher risk for cancer in general and specific cancers in particular. Studies have also suggested that restricting calories reduces the risk for cancer.
One way in which obesity may increase the risk for cancer is its association with high levels of hormones called growth factors, which can trigger rapid cell production, leading to cancer.
Associations between obesity and the following cancers have been made:
- Uterine cancer
- Breast cancer
- Prostate cancer
- Cancer of the esophagus
- Colon cancer
- Pancreatic cancer
Joints
More weight puts pressure on the bones and joints. This can lead to osteoarthritis, a disease that causes joint pain and stiffness. People who are obese are also at higher risk for carpal tunnel syndrome and other problems involving nerves in their wrists and hands.
Reproductive and Hormonal Problems
Infertility. Abnormal amounts of body fat, either 10 - 15% too high or too low, can contribute to infertility in women. Obesity is especially related to certain infertility problems, such as uterine fibroids and menstrual irregularities. In men, obesity can contribute to reduced testosterone levels and erectile dysfunction.
Effect on Pregnancy. Obesity has many dangerous effects on pregnancy. These include high blood pressure, gestational diabetes (diabetes, usually temporary, that occurs during pregnancy), urinary tract infections, blood clots, prolonged labor, and higher fetal death rate in late stages of pregnancy. Obesity is also associated with increased rates of cesarean delivery. Infants of women who are obese are also at higher risk for neural tube birth defects, which affect the brain or spine, as well as other birth defects. Folic acid supplements, ordinarily effective in preventing these conditions, may not be as protective in overweight women. Some evidence also suggests an association between obesity and stillbirths.
Effects on the Lungs
Obesity, especially moderate or severe obesity, also puts people at risk for hypoxia, a condition in which there is not enough oxygen to meet the body's needs. Obese people need to work harder to breathe. They tend to have breathing muscles and lungs that do not work as well as those in thinner people.
The Pickwickian syndrome, named for an overweight character in a Dickens novel, occurs in severe obesity when lack of oxygen produces intense and chronic sleepiness and, eventually, heart failure.
Effect on the Liver
Nonalcoholic Fatty Liver Disease. People with obesity, particularly if they also have type 2 diabetes, are at higher risk for a condition called nonalcoholic fatty liver disease, also called nonalcoholic steatohepatitis (NASH). This condition can cause liver damage that is similar to liver injury seen in alcoholism. NASH occurs in about half of people with diabetes, and 20 - 50% of obese people, depending on how severe their obesity is. NASH can also occur in overweight children.
Gallstones. The incidence of gallstones is significantly higher in obese women and men. The risk for stone formation is also high if a person loses weight too quickly. In people on ultra-low calorie diets, taking ursodeoxycholic acid (Actigall) may prevent gallstones.
Sleep Disorders
People who are obese and nap tend to fall asleep faster and sleep longer during the day. At night, however, it takes them longer to fall asleep, and they sleep less than people with normal weights. In an apparent vicious circle, studies have suggested that obesity not only interferes with sleep but that sleep problems may actually contribute to obesity.
Sleep Apnea. Obesity, particularly the apple shape, is strongly associated with sleep apnea, which occurs when the upper throat relaxes and closes from time to time during sleep. This closure temporarily blocks the passage of air. Sleep apnea is increasingly being viewed as a potentially serious health problem, which may lead to complications, such as heart disease and stroke. Obstructive sleep apnea may also increase obesity, creating a viscous cycle. Some studies indicate that treating sleep apnea may help people lose abdominal fat.
Emotional and Social Problems
Depression. Several studies have reported an association between depression and obesity, particularly in obese women. There may be a number of factors to explain the link. In some cases of atypical depression, people overeat and may gain weight. Overweight people may also become depressed because of social problems and a poor self-image. In these cases, depression usually disappears when people lose weight.
There does not appear to be any association between depression and obesity in men.
Social Problems. One long-term study reported that overweight young women completed fewer years of school, were 20% less likely to be married, and had 10% higher rates of household poverty than their thinner peers. Obese young men were also less likely to be married, and their incomes were lower than their thinner peers. Nevertheless, studies consistently show that overweight males (both boys and men) are not as severely emotionally affected as females of any age. Women and girls tend to blame themselves for being heavy, while males tend to blame being overweight on outside factors.
Health Consequences of Childhood Overweight
Children and adolescents who are overweight have poorer health than other children. Studies are reporting unhealthy cholesterol levels and high blood pressure in overweight children and adolescents. Of great concern is the dramatic increase in type 2 diabetes in young people, which is largely due to the increase in overweight children.
Weight gain in children is also linked to asthma, gallbladder problems, sleep apnea, and liver abnormalities. Overweight girls are more likely to enter puberty early, according to a new study, and subsequently be at higher risk for breast cancer. It is not clear yet how many of these childhood problems persist in people who achieve normal weight as adults. Staying overweight into adulthood certainly carries health risks.
Lifestyle Changes and Psychosocial Treatments
For most people, changing behavior takes time. All the stages of change are important. A person can learn from each stage. One can go from "not thinking about it" to "thinking about the pros and cons" to "making small changes and figuring out how to deal with the hard parts" to "doing it" to "making it part of your life." Many people fall off track and go through the stages of change several times before change really lasts.
Lifestyle changes usually involve slip-ups. People should not give up because they slip from time to time. Instead, they should forgive mistakes and get back to work toward the goal of lifelong health.
Keeping a Food Journal
A food journal is a good way to become aware of eating habits.
- Keep a food journal for 1 week. Write down what you eat, how much you eat, and what time of day you've eaten. Also write down what else you were doing and how you were feeling, such as being hungry, stressed, tired, or bored. For example, maybe you were at work and were bored, and so you got a snack from a vending machine down the hall from your desk.
- At the end of the week, review your journal and look at your eating habits. Try to decide which habits you want to change. Remember: small steps can lead to long-term success. Try not to overwhelm yourself with too many goals.
- Also, congratulate yourself for the healthy habits you do have. Many people focus on their poor habits and then become distressed and overwhelmed. Don't judge your behaviors. Setting goals to correct flaws is the best way to make new healthful habits permanent.
Think about what triggers, or prompts, may be responsible for some of your eating habits. Is there something in your environment, such as a vending machine down the hall, which makes you eat when you are not hungry or choose an unhealthy snack? Does the way you feel make you want to eat?
Look at your journal and circle the common triggers. Some of them might be:
- Seeing your favorite snack in the pantry or vending machine
- Watching television
- Feeling stressed by something at work or by another situation
- Having no plan for dinner after a long day
- Going to a staff meeting to which someone brought cupcakes
- Stopping at a fast-food restaurant for breakfast and choosing high fat, high calorie foods
- Needing a pick-me-up toward the end of your workday
Avoiding Triggers to Overeating
Start by focusing on the one or two triggers that occurred the most often during your week. Is there something you could do to avoid these triggers?
Some ways to avoid triggers are:
- Avoid walking past the vending machine to get to your desk, if possible.
- Decide what you will have for dinner early in the day so that you have a plan after work.
- Keep unhealthy snacks out of your house or negotiate with the person in your home who is buying these to keep them out of sight.
- Suggest having fruit and vegetables in place of cupcakes at staff meetings, or bring these things yourself.
Replacing old Habits with New, Healthy Ones
Some other ideas for replacing unhealthy habits with healthy ones are:
- Eat slowly. Eating too quickly leads to overeating.
- Eat only when you are hungry. Eating when you are feeling worried, tense, or bored also leads to overeating.
- Plan your meals. This reduces the chance you will buy foods you did not plan to buy (impulse buying) or eat at fast-food restaurants.
- Control your portion sizes.
- Get rid of unhealthy foods. Replace the candy dish with a fruit or nut bowl. If you must have tempting, unhealthy foods in your house for other family members, put them out of sight on a high shelf or at the back of the cupboard.
- Avoid skipping meals. Eat breakfast like a king or queen, lunch like a prince or princess, and dinner like a pauper.
It may take a while before people can turn their unhealthy habits into new, healthy ones. Since it took a while to form the old habits, it may take just as long to change them. People should not give up.
Managing Overweight Children
Childhood obesity is best treated by a non-drug, multidisciplinary approach, including diet, behavior modification, and exercise. Children should be screened for obesity at age 6, and referred to weight management programs if needed at that time. Moderate-to-intense programs have the highest rate of success with children and adolescents. These programs include counseling and behavior modifications.
Most children spend about 3 hours a day watching TV. When you add in other screen time activities, it is closer to 5 - 7 hours a day. Current screen time guidelines recommend that children under age 2 should have no screen time; above age 2, children should limit screen time to 1 - 2 hours a day.
Children should have many chances to, run, bike, and play sports during the day. Experts recommend they get 60 minutes of moderate activity every day. Moderate activity means faster breathing and faster heart beat than normal. Some examples are walking briskly, playing chase or tag, playing basketball, or playing most organized sports (such as soccer, swimming, and dancing).
Younger children have shorter attention spans than older children. They may be active for only 10 - 15 minutes at a time. The goal is still a total of 60 minutes of activity every day. These ideas may help non-athletic children become active:
- Let them know it will give them more energy, make their bodies stronger, and make them feel good about themselves.
- Encourage them to be active, so they know they can do it. They need to believe they can.
- Be their role model. If you are not active yourself, start getting more active.
- Make walking a part of your family's daily routine. All you need are good walking shoes and rain jackets for the wet days. Don't let rain stop you.
- Go for walks together after dinner, before turning on the TV or playing computer games.
- Take your family to community centers or parks where there are playgrounds, ball fields, basketball courts, and walking paths. It's easier to be active when people around you are active.
Choosing healthy snacks and drinks for your children can be a challenge. There are many to choose from.
- Put snacks in small plastic bags so they are easy to carry in a pocket or backpack. Putting snacks in small bags also helps you give your child the right size portion.
- Avoid junk-food snacks like chips, candy, cake, cookies, and ice cream. The best way to keep kids from eating junk food or other unhealthy snacks is to not have these foods in your house.
- Teach them how to avoid unhealthy foods at school.
- It's OK to let your child have an unhealthy snack once in a while. Never allowing any unhealthy snacks or sweets may result in your child sneaking these foods. The key is balance.
- Praise and reward children when they make good food choices and do healthy activities. This will encourage them to keep at it.
- Do not use food as a reward or punishment. For instance, do not offer food if your children clean their rooms, and do not withhold food if your children do not do their homework.
- Do not punish, tease, or put down children who are not motivated in their weight-loss plan. This will not motivate them.
- Do not force children to eat all the food on their plate. Infants, children, and teens need to learn to stop eating when they are full.
The best thing parents can do to motivate their kids to lose weight is to lose weight themselves, if they need to. Parents should lead the way and follow the advice they give their children.
Eating as a family is important -- having meals where everyone sits down and talks about their day. These meals should have some set rules, such as no lectures or teasing allowed. Family meals should be a positive experience. Meals should be cooked at home, and children should be involved in the meal planning. If they are old enough, they can help prepare meals.
A study in Australia, published in February 2011, found that teaching parents healthy life style skills can lead to a sustained weight reduction in moderately-obese children aged 6 - 12 years. A study published by researchers at Yale University supported this find, showing that a family lifestyle intervention produces sustained weight loss.
Support Groups and Behavioral Approaches
Commercial and Nonprofit Support Programs for Weight Loss. There are many different types of weight-loss programs. (This report cannot address all of the many commercial and nonprofit weight-loss programs currently available, nor can it assess their claims.)
Taking off Pounds Sensibly (TOPS), a nonprofit support organization with many local chapters, is one of the least expensive programs, costing about $30 a year.
Most of the commercial programs, such as Weight Watchers, Jenny Craig, and NutriSystem, offer individual or group support, lifestyle changes, and packaged meals. These programs tend to be expensive. There are few well-conducted studies on these programs.
Approach short-term specific goals regarding exercise and eating as something to learn rather than perform. Also, plan ahead when eating out or going to another home for food.
Cognitive Behavioral Approaches. Most support programs use some form of cognitive-behavioral methods to change the daily patterns associated with eating. They are very useful for preventing relapse after initial weight loss.
The patient reviews a personal diary with a therapist or group to set realistic goals and identify patterns that the patient can change. For instance, if the patient normally eats food while watching television, the patient may need to eat in another room instead.
Stress-Reduction Techniques.Stress reduction and relaxation techniques may be helpful for some people with obesity, such as those whose weight is related to night-eating syndrome.
Changing Sedentary Habits and Exercise
The weight-loss formula: calories used in exercise > calories eaten = weight loss.
This means that to lose weight, the number of calories people burn by exercising needs to be greater than the number of calories they get from what they eat and drink. Even if people work out a lot, they will gain weight if they take in more calories than they burn up.
Another way to look at this is that a 30- to 50-year-old woman who does not exercise needs about 1,800 calories a day to maintain her normal weight. A 30- to 50-year-old man who does not exercise needs about 2,200 calories to maintain his normal weight. For every hour of exercise they do, they would burn:
- 240 - 300 calories doing light activity, such as cleaning house or playing baseball or golf
- 370 - 460 calories doing moderate activity, such as a brisk walk (3.5 mph), gardening, biking (5.5 mph), or dancing.
- 580 - 730 calories doing strenuous activity, such jogging at a pace of 9 minutes per mile, playing football, or swimming laps.
- 740 - 920 calories doing very strenuous activity, such as running at a pace of 7 minutes per mile, playing racquetball, and skiing.
Even without dieting, people will lose weight if they add any of the activities above to their lifestyle.
Many people sit all day at their jobs. They can add activity to their schedule before work, during work, at lunch, and after work.
- People who drive can park around the corner or a few blocks from their work place so you get a 5- to 10-minute walk before getting to work.
- People who take the bus can get off 1 stop before their usual stop to get in a few extra minutes of walking.
- Walking or biking to work are excellent forms of exercise that will save money on parking, gas, and bus fare.
- People with sedentary jobs should set a timer to remind them to do a 1-minute stretching or strengthening exercises every half hour. These 1-minute workouts help people stay focused, and they add 16 minutes of exercise to an 8-hour workday.
- It is better to take the stairs instead of the elevator to add some exercise to the workday. It is also better to walk down the hall to talk with a coworker instead of sending an e-mail.
- People who get an hour lunch break can eat for 30 minutes, then take a 30-minute walk.
- Those who get a 30-minute lunch can try to fit in a 10-minute power walk.
People who exercise are more apt to stay on a diet plan. Exercise improves psychological well-being and replaces sedentary habits that usually lead to snacking. Exercise may even act as a mild appetite suppressant. Moreover, exercise improves overall health even with modest weight loss.
Be aware, however, that the pounds won't melt off magically. In addition, if a person exercises but doesn't diet, any actual pounds lost may be minimal. Nonetheless, regardless of weight loss, a fit body will look more toned and be healthier. In addition, exercise benefits the heart even with modest weight loss.
The following are some suggestions and observations on exercise and weight loss:
- With intense exercise, the metabolism continues to burn calories before returning to its resting level. This state of elevated metabolism can last for as little as a few minutes after light exercise to as long as several hours after prolonged or heavy exercise.
- Of the standard aerobic machines, the treadmill burns the most calories. It may be particularly effective when used in short multiple bouts during the day. In fact, frequent exercise sessions as short as 10 minutes in duration (about four times a day) may be the most successful exercise program for obese people.
- Resistance or strength training is excellent for replacing fat with muscles. It should be performed two or three times a week.
- As people slim down, their initial level of physical activity becomes easier and they burn fewer calories for the same amount of work. The rate of weight loss slows down, sometimes discouragingly so, after an initial dramatic head start using diet and exercise combinations. People should be aware of this phenomenon and keep adding to their daily exercise program.
- Changes in fat and muscle distribution may differ between men and women as they exercise. Men tend to lose abdominal fat (which lowers their risk for heart disease faster than reducing general body fat). Exercise, however, does not appear to have the same effect on weight distribution in women. In one interesting study, women in aerobic and strength training programs lost fat in their arms and trunk, but did not gain muscle tissue in these regions.
Warning Note. Because obesity is one of the risk factors for heart disease and diabetes, anyone who is overweight must discuss their exercise program with a doctor before starting. Sudden demanding exercise, in such cases, can be very dangerous.
Dietary Management
About 50 - 70 million Americans go on diets each year. No one diet is right for everyone. What works for one person may not work for another.
Before beginning a diet, look at your own eating and activity patterns. Then set goals for changing some of these patterns, or behaviors. Set goals that are realistic for you, goals that you can reach and maintain.
A good diet is one you can follow for years. It should keep your weight at a good level for you and keep you in good health. Some key features of any good weight-loss program or diet are:
- The diet should be balanced. That means eating a variety of foods, including fruits and vegetables, healthy carbohydrates, proteins, and fats.
- The diet should not be boring or keep you on the same food for long periods of time. While a weight-loss diet may take away foods you enjoy eating, you should still enjoy eating.
- Weight loss should be gradual. Claims of quick and easy sustained weight loss are rarely true. The truth is it takes time, effort, and motivation to lose weight and keep it off.
- The exact composition of a diet is generally less important than the calorie reduction it supplies.
Be cautious about any diet that makes unrealistic claims about how much weight you can expect to lose, tells you not to eat food from one of the major food groups, or is based on eating just one food or one type of food.
Keeping Track of Calories
Calorie restriction has been the cornerstone of obesity treatment. The standard dietary recommendations for losing weight are:
As a rough rule of thumb, one pound of body fat is the result of eating about 3,500 calories. A person could lose a pound a week by reducing daily caloric intake by about 500 calories a day.
To determine your daily calories requirements, multiply the number of pounds of ideal weight by 12 - 15 calories. The number of calories per pound depends on gender, age, and activity levels.
- For instance, a 50-year old woman who wants to maintain a weight of 135 pounds and is mildly active might require only 12 calories per pound (1,620 calories a day).
- A 25-year old female athlete who wants to maintain the same weight might need 25 calories per pound 2,025 (calories a day).
Fat intake should be no more than 30% of total calories. Most fats should be in the form of monounsaturated fats (such as olive oil). Saturated fats (found in animal products) should be avoided.
Warning on Extreme Diets
Extreme diets of fewer than 1,100 calories per day carry health risks and are not recommended. Most of the initial weight loss is in fluids. Later, fat is lost, but so is muscle, which can account for more than 30% of the weight loss. No one should be on very strict diets for longer than 16 weeks, or fast for weight loss.
There are a number of problems associated with extreme diets:
- They are often followed by bingeing or overeating, and a return to obesity.
- Such diets often do not supply enough vitamins and minerals, which must then be taken as supplements.
- Severe dieting has unpleasant side effects, including fatigue, dizziness, confusion, intolerance to cold, hair loss, gallstone formation, and menstrual irregularities.
- There have been rare reports of death from heart arrhythmias when liquid formulas did not have sufficient nutrients.
Pregnant women who excessively diet during the first trimester put their unborn children at risk for birth defects.
Eat A Healthy Diet to Lose Weight
Eating a balanced diet means you consume the right types and amounts of foods and drinks to keep your body healthy.
For protein in the diet, choose:
- Poultry with the skin removed
- Lean cuts of beef or pork, such as round, top sirloin, tenderloin (trim away any visible fat)
- Fish or shellfish. Although red meat does not have a specific influence on body weight, evidence suggests that a high consumption of red and processed meats is linked cancer and other serious health problems.
- Pinto beans, black beans, kidney beans, lentils, split peas, or garbanzo beans
- Nuts and seeds, including almonds, hazelnuts, mixed nuts, peanuts, peanut butter, sunflower seeds, and walnuts. But watch how much you eat.
- Tofu, tempeh, and other soy-protein products
Consume 3 cups per day of fat-free or low-fat milk or milk products. Items such as cream cheese, cream, or butter do not count as healthy dairy products.
Grain products include any food made from wheat, rice, oats, cornmeal, barley, or another cereal grain. Products made with grains include pasta, oatmeal, breads, breakfast cereals, tortillas, and grits.
Grains are divided into either whole grains or refined grains. The key to eating healthy is to choose mostly whole-grain products.
- Examples of whole grains are whole-wheat flour, bulgur (cracked wheat), oatmeal, whole cornmeal, and brown rice. To make sure you are buying or eating whole-grain products look for words such as whole grain or whole wheat.
- Refined grains have been treated to extend their shelf life and give them a finer texture. However, this process takes out fiber, iron, and many B vitamins. Limit foods that are often made with refined grains such as crackers, corn tortillas, most ready to eat cereals, white rice, and others
Oils are fats that are liquid at room temperature. Most of these oils are high in monounsaturated or polyunsaturated fats. This is the best type of oil to use in cooking or preparing foods. Solid fats are solid at room temperature. All of these contain what are called saturated fats. Saturated fats are much less healthy for your heart, blood vessels, and other parts of your body. Saturated fats often also contain cholesterol.
Eat 2 cups (4 servings) of fruit and 2 1/2 cups of vegetables (5 servings) per day for an average 2,000-calorie per day diet.
- Fruits and vegetables are low in calories. They are also packed with fiber, vitamins, and minerals. Eating a diet that is rich in fruits and vegetables can help you control your weight. It may also reduce your risk of cancer and other diseases.
- Because fruits and vegetables are high in fiber and water, they fill you up. Replace high-calorie foods with fruits and vegetables to reduce the amount of calories and fat in your diet without making you feel hungry.
Low-Carbohydrate Diets
Low carbohydrate diets generally restrict the amount of carbohydrates but do not restrict protein sources.
The Atkins diet restricts complex carbohydrates in vegetables and, particularly, fruits that are known to protect against heart disease. The Atkins diet can also cause excessive calcium excretion in the urine, which increases the risk for kidney stones and osteoporosis.
"Low-Carb" diets, such as South Beach, The Zone, and Sugar Busters, rely on a concept called the "glycemic index," or GI, which ranks foods by how fast and how high they cause blood sugar levels to rise. Foods on the lowest end of the index take longer to digest. Slow digestion wards off hunger pains. It also helps stabilize insulin levels. Foods high on the glycemic index include bread, white potatoes, and pasta, while low-glycemic foods include whole grains, fruit, lentils, and soybeans.
There has been debate about whether Atkins and other low-carbohydrate diets can increase the risk for heart disease, as people who follow these diets tend to eat more animal-saturated fat and protein and less fruits and vegetables. In general, these diets appear to lower triglyceride levels and raise HDL ("good") cholesterol levels. Total cholesterol and LDL ("bad") cholesterol levels tend to remain stable or possibly increase somewhat. However, large studies have not found an increased risk for heart disease, at least in the short term. In fact, some studies indicate that these diets may help lower blood pressure.
Low-carbohydrate diets help with weight loss in the short term, possibly better than diets that allow normal amounts of carbohydrates and restrict fats. However, overall, there is not good evidence showing long-term efficacy for these diets. Likewise, long-term safety and other possible health effects are still a concern, especially since these diets restrict healthy foods, such as fruit, vegetables, and grains while not restricting saturated fats.
Fat and Sugar Substitutes
Replacing fats and sugars with substitutes may help many people who have trouble maintaining weight.
Fat Substitutes. Fat substitutes added to commercial foods or used in baking deliver some of the desirable qualities of fat, but they do not add as many calories. They cannot be eaten in unlimited amounts, however, and are considered most useful for helping keep down total calorie count.
Olestra (Olean) passes through the body without leaving behind any calories from fat. Studies suggest that it helps improve cholesterol levels and may help overweight people lose weight. Early reports of cramps and diarrhea after eating food containing olestra have not proven to be significant. Of greater concern is the fact that even small amounts of olestra deplete the body of certain vitamins and nutrients that may help protect against serious diseases, including cancer. The FDA requires that the missing vitamins, but not other nutrients, be added back to olestra products.
Beta-glucan is a soluble fiber found in oats and barley. Products using this substance (Nu-Trim) may reduce cholesterol and have additional health benefits.
A number of other fat-replacers are also available. Although studies to date have not shown any significant adverse health effects, their effect on weight control is uncertain, since many of the products containing them may be high in sugar. People who learn to cook using foods naturally lacking or low in fat eventually lose their taste for high-fat diets, something that may not be true for those using fat substitutes.
Artificial Sweeteners. Many artificial or low-calories sweeteners are available. It should be noted that using these artificial sweeteners should not give dieters a license to increase their fat intake. There is some public concern about chemicals used to produce many of these sweeteners, and the side effects seen in studies using rats. Natural low-calories sweeteners are available that may be more acceptable to many people.
- Saccharin (Sugar Twin, Sweet'N Low, Sucaryl, and Featherweight). Saccharin has been used for years.
- Aspartame (Nutra-Sweet, Equal, and NutraTase). Aspartame has come under scrutiny because of rare reports of nervous system disorders, including headaches or dizziness, associated with its use. People with phenylketonuria (PKU), a genetic condition, should not use it. Studies have not reported any serious health dangers in otherwise healthy individuals, but some people may be sensitive to aspartame.
- Sucralose (Splenda). Sucralose has no bitter aftertaste and works well in baking, unlike other artificial sweeteners. It is made from real sugar by replacing part of the sugar with chlorine. Some people are concerned because chlorinated molecules used in major industrial chemicals have been associated with cancer and birth defects. Over 100 studies have been conducted on sucralose over a 20-year period, with no reports of such risks.
- Acesulfame-potassium (Sweet One, SwissSweet, and Sunette). It has been used in the U.S. since 1988 with no reported side effects.
- Neotame (Neotame). Neotame is a synthetic variation of aspartame, developed to avoid its side effects. The association with aspartame has raised some concerns. Studies to date have reported no effects that would cause alarm, and it appears to be safe for general consumption.
- D-tagatose (Tagatose). This reduced-calorie sweetener is made from lactose, which is the sugar found in dairy products and other foods. It may be especially beneficial for people with type 2 diabetes. It may also have additional benefits that help the intestinal tract.
- Alitame (Aclame) is formed from amino acids, the building blocks of proteins. It has the potential to be used in all products that contain sugar, including baked goods.
- Stevioside (Stevia). This is a natural sweetener derived from a South American plant. It is available in health food stores. People with diabetes should avoid alcohol-based forms. It has not been carefully tested.
Other sugar substitutes being investigated include glycyrrhizin (derived from licorice) and dihycrochalcone (derived from citrus fruits).
Liquid Meal Replacements
Some studies have reported good success with meal replacement beverages (such as Slim-Fast and Sweet Success). They contain major nutrients needed for daily requirements. Each serving typically contains 200 - 250 calories and replaces one meal. (Note: Using them for all meals reduces calories to a severe extent and can be harmful.)
These weight loss programs can cost about $2,000. People who complete these programs may lose close to 10% of their weight. For example, someone who started 200 pounds loses 20 pounds, on average. But many people regain over half of the lost weight over time.
Medications
There are several different drugs used for weight loss. Unless specifically instructed by a doctor, people should use non-drug methods for losing weight. Except under rare circumstances, pregnant or nursing women should never take diet medications of any sort, including herbal and over-the-counter remedies. While weight loss drugs in general have shown some benefit, the overall weight loss achieved is generally limited. In addition, people will usually regain the weight when they discontinue the medication.
Over-the-Counter Weight Loss Products and Herbal Remedies
About 7% of American adults use nonprescription weight-loss products. People must be cautious when using any weight-loss medications, including over-the counter diet pills and herbal remedies. Buying unverified products over the Internet can be particularly dangerous.
Green Tea. Some studies have suggested that regular tea drinking is associated with lower weight, particularly in people who drink it for years. However, better evidence is needed to confirm the results on this supplement.
Thermogenic Approach to Weight Loss. An approach to weight loss called thermogenic (or hepatothermic) therapy is based on the claim that certain natural compounds have properties that enable the liver to increase energy in cells and stimulate metabolism. Theoretically, the result would be fat loss. Among the substances used in such products are EPA-rich fish oil, sesamin, hydroxycitrate, pantethine, L-carnitine, pyruvate, aloe vera, aspartate, chromium, coenzyme Q10, green tea polyphenols, aloe vera, DHEA derivatives, cilostazol, diazoxide, and fibrate drugs.
Nearly all the current over-the-counter dietary aids contain some combination of these ingredients. There is no evidence that any of these ingredients can produce weight loss, and some may even have harmful effects.
Chromium is a common ingredient in many diet supplements (such as Xenadrine, Dexatrim, Acutrim Natural, and Twinlab Diet Fuel). It is claimed to specifically promote fat loss, rather than lean muscle loss. There is no proof that chromium helps with weight loss.
Warnings on Some Ingredients in Over-the-Counter Diet Products
Ephedra, Ephedrine, and Ma Huang. The FDA does not allow the sale of drugs that contain ephedrine. In May 2004, the FDA banned the sale of dietary supplements that contain ephedra (also called Ma Huang). Ephedra can cause serious side effects, including strokes and heart attacks.
Brazilian Diet Pill. The FDA has warned consumers not to buy a product known as the "Brazilian diet pill." This product is labeled as a dietary supplement, but contains several chemicals found in powerful prescription drugs.
Conjugated Linoleic Acid (CLA). Conjugated linoleic acid is found in many dietary products. There is no evidence that it produces weight loss. Furthermore, there is some concern that CLA might increase insulin resistance and a dangerous inflammatory response in people with obesity.
Tiratricol. Over-the-counter products containing tiratricol, a thyroid hormone, have been sold for weight loss. Such products may increase the risk for thyroid disorders, heart attack, and stroke. Tiratricol is also known as triiodothyroacetic acid or TRIAC.
Laxative Actions in Natural Substances. Many dietary herbal teas contain laxatives, which can cause gastrointestinal distress, and, if overused, may lead to chronic pain, constipation, and dependency. Rarely, dehydration and death have occurred. Some laxative substances found in teas include senna, aloe, buckthorn, rhubarb root, cascara, and castor oil.
Guar Gum. Some fiber supplements containing guar gum have also caused obstruction of the esophagus and gastrointestinal (digestive) tract.
Chitosan. Chitosan, a dietary fiber from shellfish, prevents a small amount of fat from being absorbed in the intestine. Well-conducted studies, however, have not found it to be effective. People who are allergic to shellfish should not take these supplements.
Plantain. Dietary remedies that list the ingredient plantain may contain digitalis, a powerful chemical that affects the heart. NOTE: This substance should not be confused with the harmless banana-like plant also called plantain.
Orlistat (Xenical)
Orlistat (Xenical) can help about one-third of obese patients with modest weight loss and can help in long-term maintenance of weight loss. It works by slowing the absorption of fat in the intestine (by about 30%). The average weight-loss attained is around 6 lbs. with use of this drug. However, many people regain a significant portion of this weight within 2 years. While it does not work for all patients, orlistat can improve cholesterol levels, regardless of weight loss.
Orlistat can cause gastrointestinal problems and may interfere with absorption of the fat-soluble vitamins A, D, and E and other important nutrients. The FDA recommends taking a daily multivitamin supplement when using this drug.
The most unpleasant side effect is leakage of oily feces from the anus. Restricting fats can reduce this effect. People with bowel disease should probably avoid it. In spite of these side effects, most patients are able to tolerate this medicine.
There is an approved over-the-counter version of orlistat. Sold under the name alli, it is available at half the prescription strength of Xenical. Those eager to use it should consider its cost (around $100 per month) and modest benefits compared with its side effects.
Sibutramine (Meridia)
The weight loss drug sibutramine (Meridia) has been removed from the market because of a high risk for heart attack and strokes.
Psychostimulants
Phentermine and Other Sympathomimetics. Sympathomimetics are drugs that act like the stress hormone (and chemical messenger) norepinephrine. These medications act as stimulants in the brain. Some are approved for treating obesity, but only for short-term use of 12 weeks or less. Average weight-loss has been in the range of 7 lbs. over the short-term. These medicines include:
- Phentermine (Ionamin, Adipex-P, Fastin)
- Benzphetamine (Didrex)
- Phendimetrazine (such as Adipost, Bontril, Melfiat, Plegine, Prelu-2, and Statobex)
Phentermine is the most commonly prescribed appetite suppressant, and is less expensive than orlistat or sibutramine. Its effects are not long lasting, however. It can also raise blood pressure. In addition, phentermine is associated with depression, which is already a problem in many cases of obesity. Note: Neither phentermine nor such combinations are associated with the heart problems linked to the previous phentermine combination known as Fen-Phen (phentermine and fenfluramine).
Investigative Drugs
Topiramate. Topiramate (Topamax) is an anti-seizure medication being investigated for weight reduction. Several clinical trials have reported that obese patients with type 2 diabetes given topiramate lost more weight than those receiving placebo. Weight loss was sustained for up to 1 year. The drug is also being studied for binge-eating disorders associated with obesity. However, psychiatric and neurological side effects may prevent topiramate from being used regularly.
Two weight loss drugs -- lorcaserin and Qnexa, received favorable reviews this year from FDA advisory panels. (Qnexa is a combination of topiramate and phentermine.) While the FDA is not bound by the advisory panels' decisions, it often follows them. If approved, these 2 drugs will be the first prescription weight loss drugs to go on the market since 1999, when orlistat was approved. Both lorcaserin and Qnexa were rejected in 2010 for safety concerns, but the applications were reopened following further studies and new data brought forth by the manufacturers.
Surgery
Bariatric surgeries produce weight loss through two approaches:
- Creating a smaller stomach. As a result a person will feel full or satisfied with less food and is not able to eat as much food as before.
- Rerouting the food around a portion of the small intestine that normally helps break down the food. As a result, your body will not absorb all the calories in the food you eat.
Gastric bypass (also called Roux-en-Y Gastric Bypass) creates a smaller stomach but also reroutes or bypasses a portion of the small intestine. As a result, greater weight-loss is achieved then seen with procedures that only create a smaller stomach.
These 3 surgeries above are almost always done through 5 - 6 small cuts in your belly. A camera is placed in your belly to allow the surgeon to see. This type of surgery is called laparoscopy.
Biliopancreatic diversion with a duodenal switch. BPD surgery is more complex than other weight-loss surgeries and is done much less often -- usually only for severe, morbid obesity. The surgeon removes a large portion of your stomach and re-routes where the food you eat goes, so it does not pass through most of your small intestine, where food is normally absorbed.
The care of patients undergoing bariatric surgery, before and after surgery, requires specialized expertise and facilities. Studies have shown that the likelihood of complications is significantly associated with the experience of the surgeon and staff.
Benefits of Bariatric Surgery
Patients must still develop a healthy lifestyle and be calorie conscious after weight-loss surgery. Follow-up must be lifelong. Those who are able to change their lifestyle often can expect to lose 30 to 50% of their excess weight, depending on the procedure.
Bariatric surgery can reduce the risk of disease in people who have severe obesity. These risks include diabetes, high blood pressure, heart disease, stroke, obstructive sleep apnea, arthritis, and some cancers.
Successful weight loss after surgery can also lead to improvement in those who already have these conditions.
Weighing less should also make it much easier for you to move around and do your everyday activities.
Weight-loss surgery alone is not a solution to losing weight. It can train you to eat less, but you still have to do much of the work. To lose weight and avoid complications from the procedure, you will need to follow the exercise and eating guidelines that your doctor and dietitian gave you.
Candidates for Bariatric Surgery
Surgery may be used for individuals who have severe obesity for 5 years or more and have not responded to other weight-loss therapies, such as diet, exercise, or medications.
Body mass index (BMI) is the most common measure of obesity. BMI measures your weight in relation to your height.
Doctors often use the following BMI measures to identify patients who may be most likely to benefit from weight-loss surgery:
- A BMI of 40 or greater. This usually means men are 100 pounds and women are 80 pounds over their ideal weight.
- A BMI of 35 or greater along with a serious medical condition related to obesity. These are called comorbidities, and include such conditions as:
- Diabetes (high blood sugar)
- High blood pressure
- Osteoarthritis (severe)
- Sleep apnea (symptoms such as sleepiness during the day and loud snoring, gasping, and interrupted breathing during sleep)
- Heart disease (personal or family history)
Some experts are now even encouraging weight-loss surgery for most patients with a BMI of 30 or greater and diabetes.
Your doctor must also consider medical problems that could make surgery more risky for you. These include:
- Liver or kidney disease
- Diseases of the stomach or small intestine
- Alcohol or substance abuse
- Current smoking
- Poorly controlled psychiatric or emotional problems
Patients with binge eating disorder should be identified before surgery and treated. A full evaluation, including a psychological evaluation, should be performed on all candidates for surgery.
Depending on insurance coverage and which procedure is performed, the cost of bariatric surgery may be up to $35,000. More and more insurance companies are willing to pay for the surgeries for patients who meet the above criteria.
Patient considering bariatric surgery should be well-informed regarding the procedure, its efficacy, side effects, and complications. They should also understand the following:
- Lifestyle and behavioral changes will still be needed after surgery, including:
- The continued need to focus on weight
- The need to chew food well
- The need for dietary restrictions
- The need for vitamin and mineral supplementation
- Patients will be unable to eat large meals.
- Surgery may not be successful in achieving significant weight loss.
Is weight-loss surgery safe for teens?
- Studies about adolescents who have had bariatric surgery suggest that these operations are at least as safe for adolescents as they are for adults. But not enough teenagers have been followed after their weight-loss surgery to know if there are any long-term effects on their future growth or development.
- Teenagers' bodies are still changing and developing. Because of the quick weight loss after surgery, they will need to be careful to get all of the nutrients and vitamins their bodies require.
- Because gastric bypass surgery changes the way some nutrients are absorbed, teens who have weight-loss surgery will need to take certain vitamins and minerals for the rest of their life.
Laparoscopic gastric banding
In laparoscopic gastric banding, the surgeon places a band around the upper part of the stomach to create a small pouch to hold food. After surgery, the doctor can adjust the band to make food pass more slowly or quickly through your digestive system. The band around your stomach is filled with saline (saltwater). It is connected to a container (access port) that is placed under your skin in your upper belly. Your surgeon can make the band tighter or looser by increasing or decreasing the amount of saline in the band. To do this, your surgeon will insert a needle through your skin into the access port.
Most people go home the same day of surgery. Some will stay one night in the hospital. Most people take 1 week off of work.
The average weight loss is about one-third to one-half of the extra weight you are carrying. This may be enough for many patients. The weight will usually come off more slowly than with gastric bypass. You should keep losing weight for up to 3 years.
The band is removable, if necessary. Studies to date indicate that the intestinal tract returns to normal afterward. Studies, including those done in the elderly, have reported significant weight loss and improved quality of life with the procedure.
Gastric Bypass
In gastric bypass, the stomach is divided with staples into two parts. The first part is very small, about the size of a golf ball. This small stomach is called the pouch. The second part of the stomach is much bigger, but food cannot go into it.
The small intestine is connected to the small pouch, which re-routes food around the big part of the stomach. The pouch can only hold a small amount of food, so if you eat too much or too fast you will throw up. Also, your body will not absorb all the calories in the food you eat.
Most people stay in the hospital for 2 days after open surgery. Patients may have a drain (tube) coming out of the stomach, which will drain fluids that build up after surgery. The drain tube is usually taken out about 7 - 10 days after surgery.
People may need to take time off from work for 3 - 4 weeks. However, if the work does not involve too much physical activity, they may be able to return to work sooner.
Total weight loss after bypass surgery is usually greater than after gastric banding.
Vertical Sleeve Gastrectomy (Gastric Sleeve)
This surgery has most often been done on patients who are too heavy to safely have other types of weight-loss surgery. Some patients who have this surgery may need a second weight-loss surgery at some time in the future.
In the gastric sleeve surgery, a large portion of the stomach is removed. The new, smaller stomach is about the size of a banana. It limits the amount of food a person can eat by making them feel full after eating only small amounts.
Most people can go home 2 days after the surgery. Patients should be able to drink clear liquids on the day after surgery, and eat a puréed diet by the time they go home.
The final weight loss may not be as large as with gastric bypass. However, it may be enough for many patients. Because vertical sleeve gastrectomy is a newer procedure, there is less data about the long-term benefits and risks. Patients should consult with their doctor about which procedure is best for them.
Weight will usually come off more slowly after gastric sleeve surgery than after gastric bypass. Patients should keep losing weight for up to 2 - 3 years.
Side Effects and Complications
Risks common to all weight-loss surgeries are:
- Gallstones and gallbladder attacks -- these occur more often from rapid weight loss.
- Gastritis (inflamed stomach lining), heartburn, or stomach ulcers.
- Depression
- Injury to your stomach, intestines, or other organs during surgery.
- Poor nutrition -- patients will eat less food after surgery, and their body will not absorb all the calories, protein, vitamins, and minerals from the food they eat.
- Scarring inside your belly -- this could lead to a bowel obstruction (blockage) in the future.
- Vomiting -- from eating more than the stomach pouch can hold.
These problems with a gastric band or access port may occur:
- The gastric band may slip partly out of place.
- The gastric band may erode into the wall of the stomach.
- The band may cause heartburn or reflux symptoms.
- The port or tubing may break or leak. Fixing this problem would require a minor operation.
These problems may occur after gastric bypass:
- A leak can occur from any of the staple lines or from where the intestine is re-connected. If a leak occurs you most likely need surgery to repair the leak. The risk of a leak is about 1%.
- The opening between the stomach pouch and your small intestine may get narrower. This is called a stricture. This can be treated by placing a scope down the patient's throat and using a balloon to stretch the opening bigger. Surgery is rarely needed to fix this problem.
- Open surgery may lead to an incisional hernia. An incisional hernia is a bulging of tissue through the incision.
- Anemia -- from low iron or vitamin B12 levels.
- Dumping syndrome -- this is when the contents in the stomach move through the small intestine quickly. It causes discomfort.
- Kidney stones
- Thinning of the bones (osteoporosis) -- due to the body absorbing less vitamin D and calcium.
- Patients who do not take enough protein after surgery can become malnourished.
After vertical sleeve gastrectomy, stomach contents may leak from where the remaining parts of the stomach are stapled together. Patients may need another operation to repair this problem if it occurs.
Care after Bariatric Procedures
Most people stay in the hospital for a few days after gastric bypass surgery. Patients are discharged when they can:
- Eat liquid or pureed food without vomiting.
- Move without too much discomfort.
- No longer need pain medication given by injection.
Patients continue to eat a liquid or soft diet for several weeks after the surgery. In patients receiving a pouch procedure, the pouch eventually expands to about one cup of chewed food (a normal stomach can hold up to one quart).
Follow-up appointments are essential to determine if nutritional supplements, such as iron, calcium, vitamin B12, or other nutrients, are needed. Supplements, such as a multivitamin with minerals, may be prescribed.
Patients should eat small meals (usually six) throughout the day, rather than large meals that the stomach can no longer handle.
The new stomach probably won't be able to handle both solid food and fluids at the same time. Patients should separate fluid and food intake by at least 30 minutes and only sip what they are drinking.
After surgery, tolerance of fat, alcohol, or sugar decreases. Patients should reduce their fat intake, especially:
- Deep-fried foods
- Fast-food meals
- High-fat foods
- High-sugar foods, such as cakes, cookies, and candy
Exercise and the support of others (for example, joining a support group with people who have undergone weight-loss surgery) are extremely important in achieving and maintaining weight loss after bariatric surgery.
Exercising can usually resume 6 weeks after the operation. Even sooner than that, most patients will be able to take short walks at a comfortable pace, after consulting with their doctor.
Resources
- www.healthierus.gov/dietaryguidelines -- Dietary Guidelines for Americans 2005
- www.eatright.org -- American Dietetic Association
- www.nutrition.gov. -- Nutrition.gov
- www.asbs.org -- American Society for Bariatric Surgery
- www.cnpp.usda.gov -- Center for Nutrition Policy and Promotion
- http://fnic.nal.usda.gov -- Food and Nutrition Information Center
- www.heart.org -- American Heart Association
- www.nationaleatingdisorders.org -- National Eating Disorders Organization
- www.fda.gov -- Food and Drug Administration
- http://win.niddk.nih.gov -- Weight-Control Information Network
References
Bessesen DH. Update on obesity. J Clin Endocrinol Metab. 2008;93(6):2027-2034.
Blackburn GL, Hutter MM, Harvey AM, et al. Expert panel on weight loss surgery: executive report update. Obesity(Silver Spring). 2009;17(5):842-862.
Barnett SJ. Contemporary surgical management of the obese adolescent. Curr Opin Pediatr. 2011;23(3):351-5.
Centers for Disease Control and Prevention. Tips for parents -- Ideas to help children maintain a healthy weight. Updated May 19, 2009. Available online.
Centers for Disease Control and Prevention. 2010 Overweight and Obesity -- Defining Overweight and Obesity. Available online.
Chu SY, Kim, Lau J, et al. Maternal obesity and risk of stillbirth: a meta analysis. Am J Obstet Gynecol. 2007;197(3):223-8.
DeMaria EJ. Bariatric surgery for morbid obesity. N Engl J Med. 2007;356(21): 2176-2183.
Dixon JB, O'Brien PE, Playfair J, et al. Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA. 2008;299(3):316-323.
Egberts K, Brown WA, O'Brien PE. Systematic review of erosion after laparoscopic adjustable gastric banding. Obes Surg. 2011;21(8):1272-9.
Flegal KM, Caroll MD, Ogden CL, Curtin LR. Prevalence and Trends in Obesity Among US Adults, 1999-2008. JAMA. 2010;303(3):235-241
Gadde KM, Allison DB, Ryan DH, et al. Effects of low-dose, controlled-release, phentermine plus topiramate combination on weight and associated comorbidities in overweight and obese adults (CONQUER): a randomised, placebo-controlled, phase 3 trial. The Lancet. 2011;377(9774):1341-1352.
Garb J, Welch G, Zagarins S, Kuhn J, Romanelli J. Bariatric surgery for the treatment of morbid obesity: a meta-analysis of weight loss outcomes for laparoscopic adjustable gastric banding and laparoscopic gastric bypass. Obes Surg. 2009;19(10):1447-1455.
Gardner CD, Kiazand A, Alhassan S, et al. Comparison of the Atkins, Zone, Ornish, and LEARN diets for change in weight and related risk factors among overweight premenopausal women: the A TO Z Weight Loss Study: a randomized trial. JAMA. 2007;297(9): 969-977.
Garvey WT, Ryan DH, Look M, Gadde KM, Allison DB, Peterson CA, et al. Two-year sustained weight loss and metabolic benefits with controlled-release phentermine/topiramate in obese and overweight adults (SEQUEL): a randomized, placebo-controlled, phase 3 extension study. Am J Clin Nutr. 2012;95(2):297-308.
Hsing AW, Sakoda LC, Chua S Jr. Obesity, metabolic syndrome, and prostate cancer. Am J Clin Nutr. 2007;86(3):s843-857.
Hughes AR, Stewart L, Chapple J, et al. Randomized, controlled trial of a best-practice individualized behavioral program for treatment of childhood overweight: Scottish Childhood Overweight Treatment Trial (SCOTT). Pediatrics. 2008;121(3):e539-546.
International Diabetes Federation. Bariatric Surgical and Procedural Interventions in the Treatment of Obese Patients with Type 2 Diabetes: A position statement from the International Diabetes Federation Taskforce on Epidemiology and Prevention. 3/28/2011. Available online.
Jolly K, Lewis A, Beach J, Denley J, Adab P, Deeks JJ, et al. Comparison of range of commercial or primary care led weight reduction programmes with minimal intervention control for weight loss in obesity: lighten Up randomised controlled trial. BMJ. 2011;343:d6500
Meijer RI, van Wagensveld BA, Siegert CE, Eringa EC, Serné EH, Smulders YM. Bariatric surgery as a novel
treatment for type 2 diabetes mellitus: a systematic review. Arch Surg. 2011;146(6):744-50.
Magarey AM, Perry RA, Baur, LA, et al. A Parent-Led Family-Focused Treatment Program for Overweight Children Aged 5 to 9 Years: The PEACH RCT. Pediatrics. 2011;127(2):214-222.
Mustelin L, Silventoinen K, Pietiläinen K, Rissanen A, Kaprio J. Physical activity reduces the influence of genetic effects on BMI and waist circumference: a study in young adult twins. Int J Obes (Lond). 2009;33(1):29-36.
O'Brien PE, Sawyer SM, Laurie C, et al. Laparoscopic adjustable gastric banding in severely obese adolescents: a randomized trial. JAMA. 2010;303(6):519-526. Erratum in: JAMA. 2010;303(23):2357.
Rosenstock J, Hollander P, Gadde KM, et al. A randomized, double-blind, placebo-controlled, multicenter study to assess the efficacy and safety of topiramate controlled release in the treatment of obese type 2 diabetic patients. Diabetes Care. 2007;30(6):1480-1486.
Stothard KJ, Tennant PW, Bell R, Rankin J. Maternal overweight and obesity and the risk of congenital anomalies: a systematic review and meta-analysis. JAMA. 2009;301(6):636-650.
Svetke, LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA. 2008;299(10):1139-48.
U.S. Department of Agriculture, Center for Nutrition Policy and Promotion. Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, 2010. Available online.
US Preventive Services Task Force. Screening for Obesity in Children and Adolescents: US Preventive Services Task Force Recommendation Statement. Pediatrics. 2010;125;361-367; originally published online Jan 18, 2010.
Wahi G, Parkin PC, Beyene J, Uleryk EM, Birken CS. Effectiveness of interventions aimed at reducing screen time in children: a systematic review and meta-analysis of randomized controlled trials. Arch Pediatr Adolesc Med. 2011;165(11):979-86.
Wardle J, Carnell S, Haworth CM, et al. Evidence for a strong genetic influence on childhood adiposity despite the force of the obesogenic environment. Am J Clin Nutr. 2008;87(2):398-404.
Woo JG, Dolan LM, Morrow AL, et al. Breastfeeding helps explain racial and socioeconomic status disparities in adolescent adiposity. Pediatrics. 2008;121(3):e458-65.
|
Review Date:
5/27/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |











